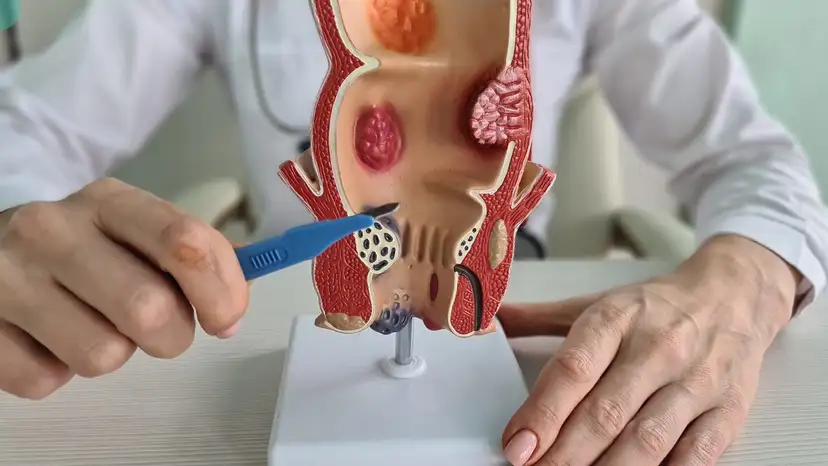
Anal fistulas are abnormal connections that form between the anal canal and the skin near the anus. They often result from infections in the anal glands and can lead to persistent discomfort, swelling, or discharge. People with anal fistulas frequently experience pain during bowel movements, itching, and irritation that affect their daily activities. If left untreated, fistulas can cause recurrent infections and chronic discomfort, making long-term symptom control difficult. Understanding the condition is crucial for deciding on the right treatment approach. Anal fistulas can vary in complexity and may involve multiple tracts, which influences the choice of surgical repair. Recognizing early signs such as pus drainage, swelling, or intermittent pain can help individuals seek medical attention before complications worsen.
Treatment for anal fistulas depends on the severity and type of fistula. Non-surgical management is sometimes possible for small or uncomplicated fistulas and may include antibiotics, anti-inflammatory medications, and meticulous hygiene practices. Warm baths and sitz baths can also relieve discomfort and reduce inflammation. However, most persistent fistulas require surgical intervention for effective long-term symptom control. The main surgical options aim to remove the fistula tract, promote healing, and preserve the anal sphincter function. Choosing between these options depends on factors such as the fistula’s location, size, and involvement of the anal sphincter muscles. Understanding all available options empowers patients to make informed decisions and manage their expectations regarding recovery and outcomes.
Anal fistula repair and removal primarily involve two surgical techniques: fistulotomy and fistulectomy. Fistulotomy involves opening the fistula tract to allow it to heal from the inside out. This procedure is effective for superficial and straightforward fistulas and typically has a shorter recovery time. Fistulectomy, on the other hand, involves complete excision of the fistula tract. It is often preferred for more complex or recurrent fistulas but may require a longer recovery period. Factors influencing the choice between fistulotomy and fistulectomy include the risk of incontinence, complexity of the fistula, and previous treatments. Consulting with a colorectal surgeon ensures the procedure is tailored to individual needs and maximizes long-term symptom control. Both procedures aim to remove the source of infection, promote healing, and reduce the risk of recurrence while minimizing complications.
Recovery after anal fistula surgery requires careful attention to postoperative care. Pain management is an important aspect and may include prescribed medications and over-the-counter pain relievers. Wound care is critical to prevent infection and promote proper healing, including keeping the area clean and dry. Patients are usually advised to take sitz baths several times a day and after bowel movements. Activity restrictions are recommended during the initial recovery phase to prevent strain on the surgical site. Regular follow-up appointments allow the surgeon to monitor healing and address any complications early. Dietary modifications, such as consuming high-fiber foods and staying hydrated, help prevent constipation and reduce pressure on the anal area. Recovery timelines can vary depending on the procedure, with fistulotomy often requiring a few weeks and fistulectomy taking longer.
Long-term symptom control involves adopting strategies to maintain anal health and reduce the risk of recurrence. Proper hygiene practices, including gentle cleaning and avoiding harsh soaps, are essential. Eating a fiber-rich diet and drinking plenty of water helps ensure smooth bowel movements. Avoiding prolonged sitting and incorporating regular physical activity can improve circulation and support healing. Patients should monitor for signs of recurrence, such as persistent discharge or new pain, and report them promptly to their healthcare provider. Regular check-ups with a colorectal specialist help identify any complications early. Understanding the importance of lifestyle adjustments empowers patients to take an active role in their recovery and long-term symptom management.
Choosing the right specialist is critical for successful anal fistula repair and removal. Colorectal surgeons with extensive experience in fistula repair provide personalized treatment plans based on the complexity of the condition. It is important to ask questions about procedure options, expected recovery timelines, and potential risks. Seeking a second opinion can provide reassurance and additional insight into the most suitable surgical approach. Patients should verify the surgeon’s experience with both fistulotomy and fistulectomy and discuss how these procedures affect sphincter function. Building a trusting relationship with the specialist enhances communication and ensures that patients feel supported throughout the treatment process. Knowledgeable specialists can also offer guidance on postoperative care and lifestyle adjustments to support long-term symptom control.
Patients undergoing anal fistula repair often benefit from understanding realistic outcomes and preparing for the recovery process. Managing expectations about healing timelines and temporary discomfort reduces anxiety. Support from family or caregivers can make daily care and wound management easier. Some patients may experience minor complications, such as temporary incontinence or delayed healing, which usually improve with proper care. Learning about coping strategies for pain and hygiene helps maintain comfort and prevent infection. Symptom control improves over time as the surgical site heals and the risk of recurrence decreases. Awareness of these factors empowers patients to participate actively in their treatment and recovery journey.
Frequently Asked Questions
How long does it take to fully recover after anal fistula surgery
Recovery varies depending on the type of procedure and complexity of the fistula. Fistulotomy typically requires two to six weeks, while fistulectomy may take six to twelve weeks.
What are the risks of fistulotomy versus fistulectomy
Fistulotomy is generally less invasive with a lower risk of incontinence, while fistulectomy may have a higher risk of complications but can be more effective for complex fistulas.
Can anal fistulas heal without surgery
Small and uncomplicated fistulas may sometimes heal with non-surgical management, but persistent or complex fistulas usually require surgical intervention.
How likely is a fistula to recur after repair
Recurrence depends on fistula complexity, surgical technique, and adherence to postoperative care. Proper follow-up and lifestyle adjustments reduce the risk of recurrence.
Are there lifestyle changes that help prevent fistula formation
Maintaining anal hygiene, consuming a high-fiber diet, staying hydrated, avoiding prolonged sitting, and regular physical activity can support anal health and reduce recurrence.
Takeaway
Anal fistula repair and removal provide effective long-term symptom control when tailored to the individual and supported by proper postoperative care. Choosing the right surgical procedure, following wound care guidelines, adopting healthy lifestyle practices, and maintaining regular follow-ups are essential to achieving optimal outcomes. Patients can regain comfort, improve quality of life, and significantly reduce the risk of recurrence by understanding their condition, actively participating in their recovery, and seeking expert care.